Care home staff will be required to have coronavirus vaccinations “to protect residents” and making jabs compulsory for people in the NHS is also being considered.
Health Secretary Matt Hancock confirmed the move on care homes in England despite the strong concerns expressed by sector leaders around the impact it could have on already-stretched staffing levels.
He told Parliament that “after careful consultation we’ve decided to take this proposal forward to protect residents”.
He said a consultation will be had on the same approach in the NHS “to save lives and protect patients from disease”.
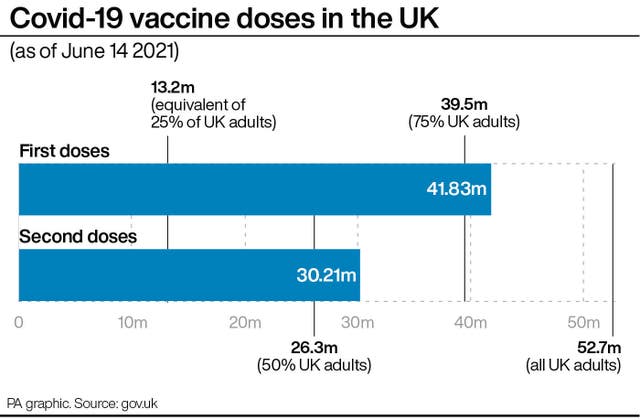
Speaking in the Commons, he said: “The vast majority of staff in care homes are already vaccinated but not all, and we know that the vaccine not only protects you but protects those around you.
“Therefore we will be taking forward the measures to ensure the mandation as a condition of deployment for staff in care homes and we will consult on the same approach in the NHS in order to save lives and protect patients from disease.”
England’s chief medical officer, Professor Chris Whitty, has previously said doctors and care workers have a “professional responsibility” to protect their patients.
From October, subject to parliamentary approval and a 16-week grace period, anyone working in a Care Quality Commission-registered care home in England must have two doses of a Covid-19 vaccine unless they have a medical exemption, the Department of Health and Social Care said.
The requirement will also apply to people coming into care homes to do other work, such as tradespeople, hairdressers and beauticians, and inspectors.
There will be exceptions for family and friends visiting care homes, under 18s, emergency services and people undertaking urgent maintenance work, the department said.
The new rules follow what the department described as an extensive consultation with the social care sector, staff, residents and their families, which garnered more than 13,500 responses.
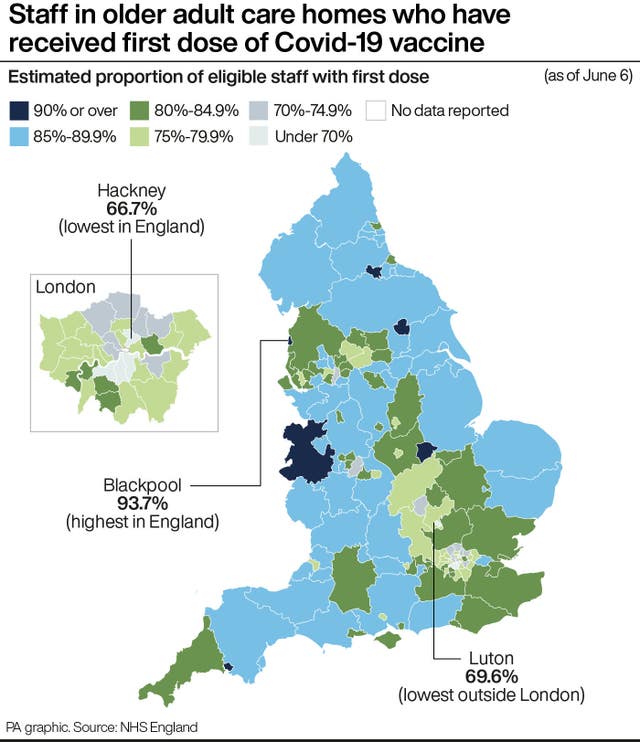
They come amid concerns that some parts of the country, such as London, have particularly low uptake of vaccines for care home staff.
NHS figures to June 6 show overall that 84% of staff in older adult care homes in England have had one dose of vaccine, and almost 69% have had both jabs.
But the data show that in Hackney, east London, for example, just 66.7% of staff in older adult care homes have had their first dose, with only 58.6% of staff in the borough having both doses.
Although the majority of care home workers have now been jabbed, only 65% of care homes with older residents in England are currently meeting the minimum level of staff uptake for one dose needed to reduce the risk of outbreaks – falling to 44% of care homes in London, the department said.
It said the social care working group of the Scientific Advisory Group for Emergencies (Sage) has advised that an uptake rate for one dose of 80% in staff in each care home setting is required for the minimum level of protection against outbreaks of the virus.
However, the move to make jabs compulsory is controversial, with the GMB union claiming more than a third of carers would consider leaving their jobs because of it.
Some care home staff have already signalled as such, according to one operator in the sector.
Geoff Butcher, who runs six homes in the Midlands, said he also knows of someone who has now decided not to get the jab “on principle”, and another who walked out of a job interview because of reports it is to be made mandatory.
He told the PA news agency that staffing issues are the “biggest concern” for the sector and that the Government move “will add hugely to the problems in recruiting”.
Dr Susan Hopkins, strategic response director for Covid-19 at Public Health England, said there are “pros and cons to any debate on mandatory vaccination”, and told the Science and Technology Committee ahead of the announcement that she would “remain a little bit concerned that we will have shortages of care staff once the mandate has come in”.
Mike Padgham, chairman of the Independent Care Group (ICG) which represents care homes in Yorkshire, said recruitment was “always challenging” before the pandemic and “is becoming more critical now”.
He told PA the move could deter people from taking on a care home job, and see those already in work leave because of the decision, adding: “I think people will be put off”.
The department acknowledged the issue of whether or not to make coronavirus and flu vaccination a condition of deployment in the NHS is “complex” and said the Government will be looking for a wide range of perspectives from across the sector for its public consultation, which will be launched “in due course”.
NHS Providers, the body representing health trusts, said compulsory vaccination “raises a range of complex employment, legal, ethical, and practical questions for trusts” and welcomed the launch of a formal consultation.
The organisation’s deputy chief executive, Saffron Cordery, said there are “different views” on the issue and said many trust leaders “will ask whether the introduction of mandatory vaccination for the flu and Covid-19 jab for NHS staff is the right approach to take at this point”.
She said: “There are alternative approaches – such as continuing to invest in individual conversations and requiring a flu or covid-19 injection as a condition of employment for all new entrants to the NHS. This is, of course, very different to retrospectively imposing this condition for all existing employees.
“Trust leaders are clear that, if the government does proceed, it will need to fully think through the consequences of mandation, including the need for trusts, if required, to potentially suspend and dismiss staff who refuse to have a vaccination at a time when the NHS already has significant vacancy rates”.
Dr Chaand Nagpaul, BMA council chair, said mandatory vaccination for NHS staff is “an incredibly complex issue that raises many ethical, legal and practical questions”, adding that the BMA will discuss the issue with its members and respond in full to the consultation.
He said: “Vaccine uptake among doctors remains high. But as we have said previously, where fewer members of staff have been vaccinated, there must be an understanding of why this is so.
“Vaccine hesitancy is not the same as flat-out refusal, and there could be several reasons why some staff may be unable or unwilling to be vaccinated.
“Doctors naturally want to be protected against this potentially lethal infection that has already taken far too many lives, including hundreds of their colleagues’, so those who do decline a vaccine are unlikely to do so lightly.
“Compulsion is a blunt instrument to tackle a complex issue.
“Recent research has highlighted that pressurising health and social care workers can have damaging effects, leading to an erosion of trust, worsening concerns about the vaccine and hardened stances on declining vaccination.”
He said the fact there appears to be lower uptake among people from certain ethnic backgrounds needs “serious consideration”, adding that any policy on mandatory vaccination for staff must not be discriminatory.
“Therefore, efforts should be focused on targeted engagement and possible alternative mitigations against transmission for those who are not vaccinated – something that has been reinforced in recent NHS England guidance.
“Crucially, doctors who have faced such a gruelling year, and may have given decades of their lives to the NHS, must not now or in future face losing their jobs for declining a vaccine,” he said.




Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel